Professor Sir David Warrell

Contact information
Research groups
Colleges
WHO SEARO Guidelines for the management of snake-bites. WHO Regional Office for South-East Asia, 3rd Ed 2016.
David Warrell
DM, DSc, FRCP, FRCPE, FMedSci; HonF CeylonCP, RThaiCP, WestAfrCP, CPSMumbai
Emeritus Professor of Tropical Medicine
- Honorary Fellow of St Cross College, University of Oxford
- Founding Director Emeritus, Oxford Tropical Medicine Network
- Principal Fellow, Australian Venom Research Unit, Department of Pharmacology and Therapeutics, University of Melbourne
- Hon Prof Tropical Medicine, University of Medicine-1, Yangon, Myanmar
- Profesor Honorario Universidad Nacional Mayor de San Marcos, Lima, Peru
- Professor Emeritus, Gorgas Institute, Universidad Peruana, Cayetano Heredia, Lima, Peru
- International Advisor, Australian DFAT-GPFD Myanmar Snake-bite Project, University of Adelaide
- Core Adviser and Editor, WHO Snakebite Envenoming Working Group (SBE-WG)
Global Snakebite Initiative
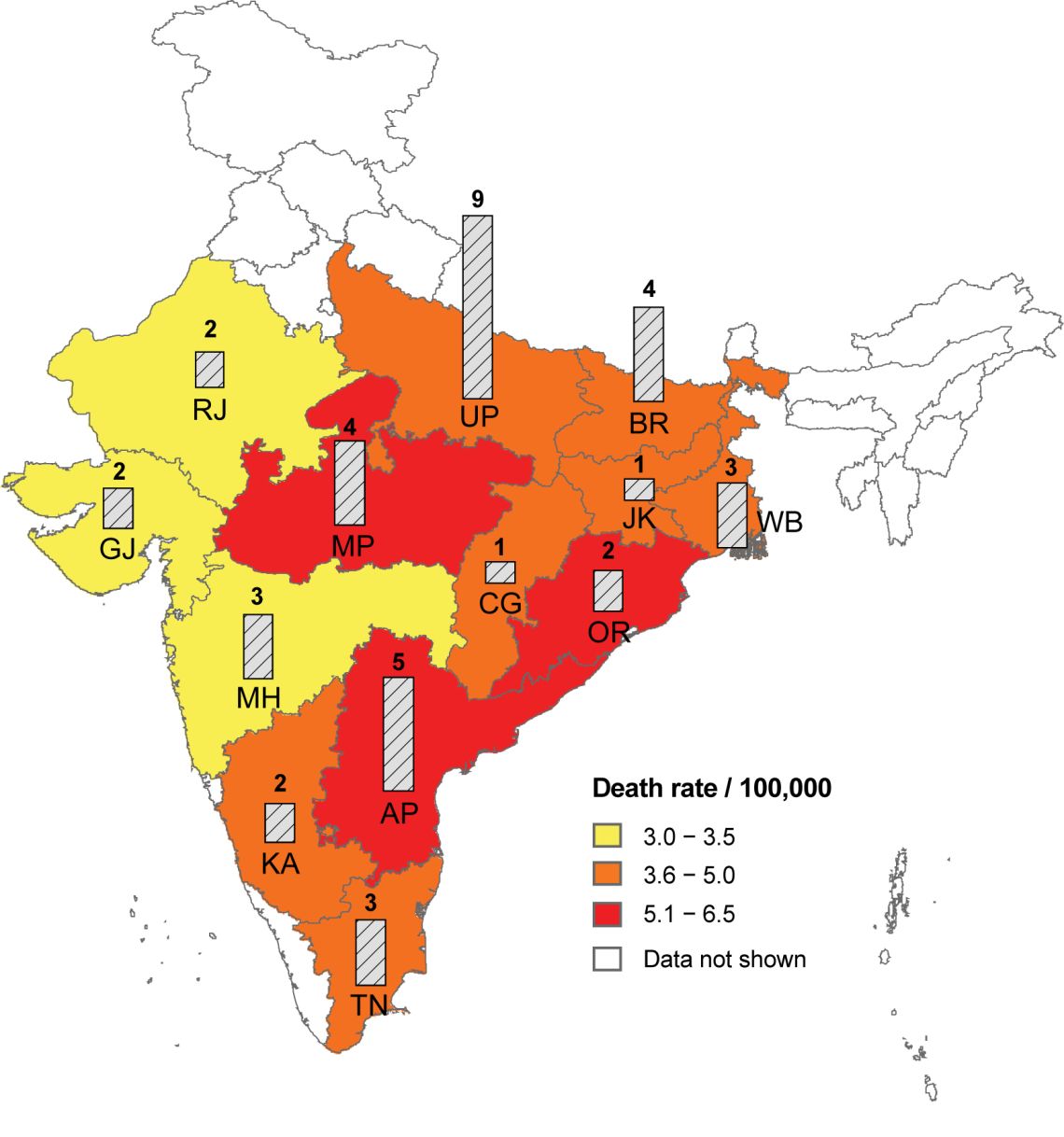
Research on the incidence, morbidity and mortality of snake bites in Africa, Asia, Oceania and Latin America; and on the clinical presentation, pathophysiology, treatment and prevention of envenoming by snakes and other venomous animals. Current sites of active research are Myanmar and Papua New Guinea. The key component of snake bite treatment is provision of specific antivenom. New antivenoms for treatment of saw-scaled viper bites in Nigeria and of taipan bites in Papua New Guinea have been developed and have been clinically tested. Recent findings in India give support to the belief that snake bite is the most neglected of all the neglected tropical diseases (NTDs) and deserves reprioritisation. This programme is aimed at producing evidence relevant to establishing the true status of snake bite as a public health problem. It has succeeded so far in: 1-persuading WHO to reinsert snake-bite into its list of NTDs with category A prioritisation; 2-introducing snake-bite onto the main agenda of the WHO World Health Assembly (May 2018); 3-coordinating a multi-disciplinary approach to studies of venomous snakes, their venoms and the clinical management of snake-bite.
Professor Warrel was appointed Knight Commander of the Order of St Michael and St George for services to global Health Research and Clinical Practice at the Queen's Birthday Honours in 2022
Recent publications
-
Correspondence Letter to the editor: Comment on "Acute kidney injury, coagulopathy, and deep vein thrombosis following a haemotoxic snakebite: A case report from a resource-limited setting." (Asaduzzaman et al., 2025).
Journal article
Warrell DA., (2025), Toxicon : official journal of the International Society on Toxinology
-
Medically important snakes and snakebite envenoming in Iran.
Journal article
Dehghani R. et al, (2023), Toxicon
-
Clinical aspects of snakebite envenoming and its treatment in low-resource settings.
Journal article
Warrell DA. and Williams DJ., (2023), Lancet
-
A case of envenoming by a Persian false-horned viper Pseudocerastes persicus (Duméril, Bibron & Duméril, 1854) (Serpentes: Viperidae) in Southeastern Iran.
Journal article
Kazemi SM. et al, (2022), Toxicon, 223
-
A case series of samar cobra, Naja samarensis peters, 1861 (Elapidae) envenomation.
Journal article
Paghubasan J. et al, (2022), Toxicon : official journal of the International Society on Toxinology



 ©
David A. Warrell
©
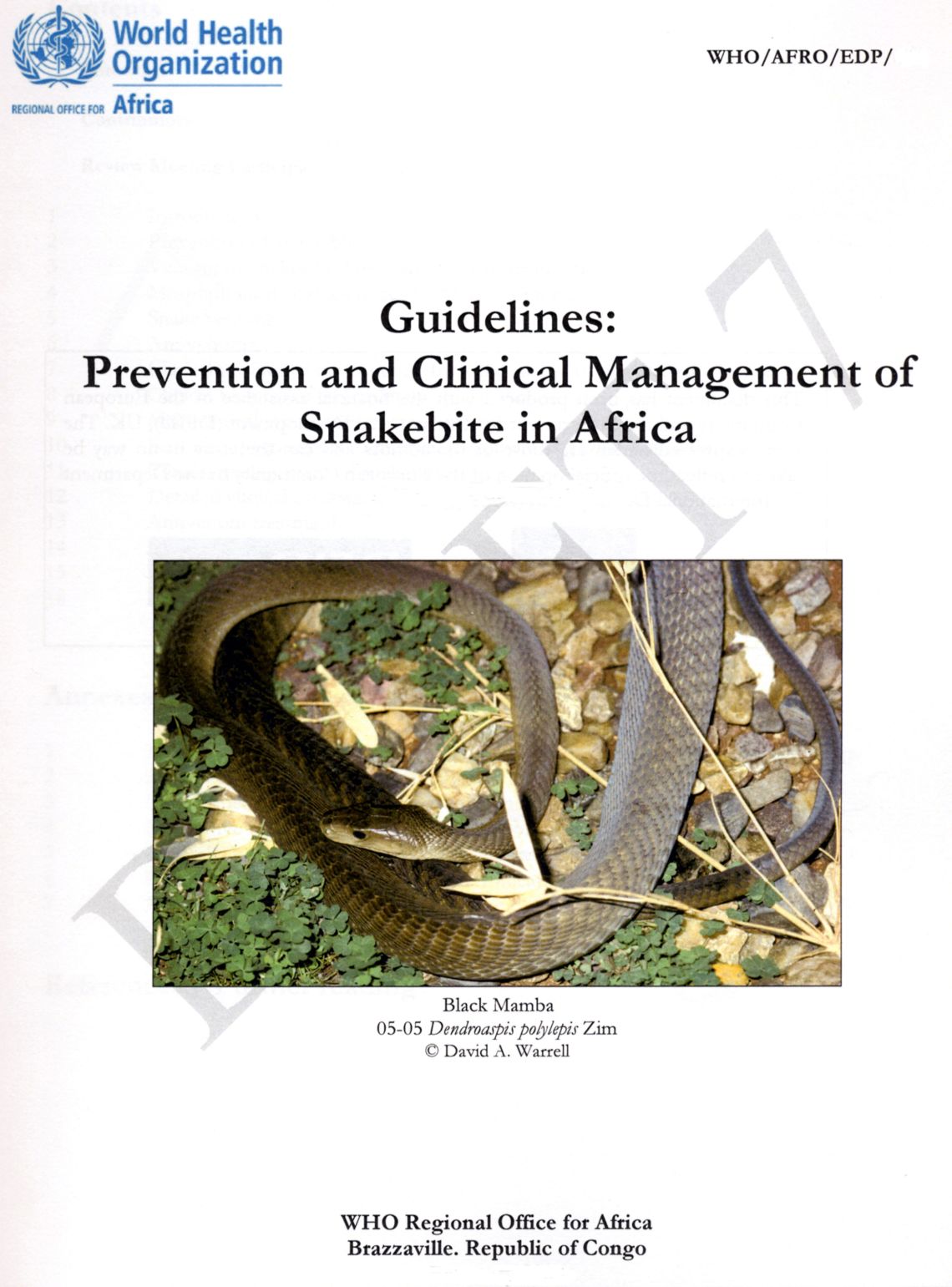
David A. Warrell