Professor Joel Tarning

Contact information
Podcast interview
Getting the dose right

Too high a dose can result in toxicity and side-effects, too low a dose can cause the illness to come back and at worse develop resistance. In the case of malaria, it is particularly important to get the dosage right for more vulnerable patients such as children and pregnant women. Professor Joel Tarning's findings have now been adopted by the World Health Organisation.
Research groups
Joel Tarning
Professor of Clinical Pharmacology
Clinical Pharmacology
Joel Tarning is the head of the Clinical Pharmacology group focusing on bioanlytical method development, drug measurements in biological fluids and pharmacometric research. His research interest includes dose-optimisation using novel pharmacometric modelling approaches. His particular research interest includes antimalarial treatment in children and pregnant women.
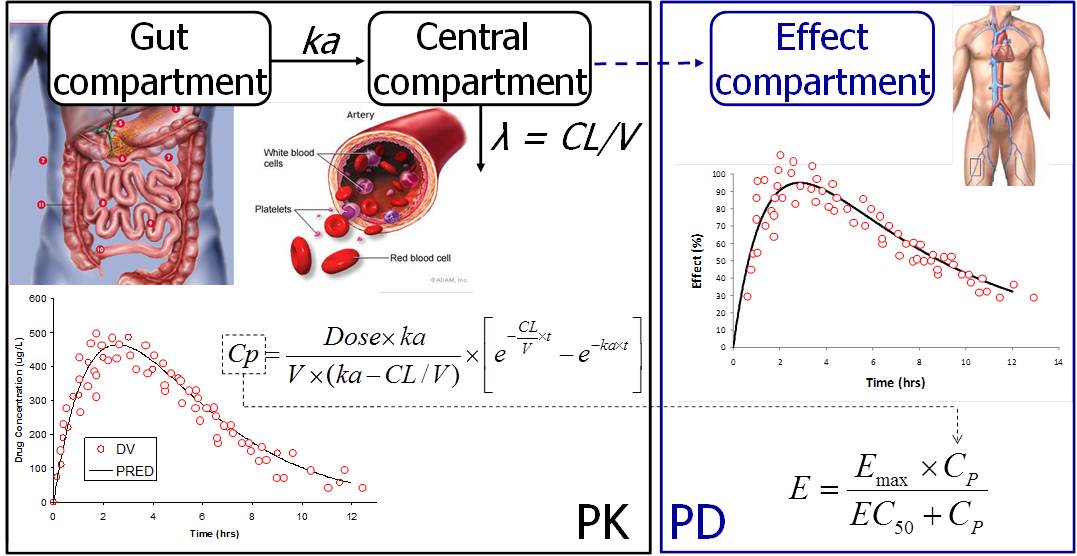
The only way to determine accurately the correct dose regimens for antimalarial treatment is to establish a dose-response relationship through pharmacokinetic (PK) and pharmacodynamic (PD) modelling. Our research has shown that many of the antimalarial drugs developed in the past fifty years were introduced at the wrong dose, particularly in young children and pregnant women. This undoubtedly contributed to therapeutic failures and the development of drug-resistant parasites. Improving existing treatments and ensuring optimal dosing of the new drugs is essential for success in the control and elimination of malaria.
Joel Tarning received the biennial Giorgio Segré Prize from EUFEPS in 2014 for his research on the pharmacokinetic and pharmacodynamic properties of antimalarial drugs in vulnerable populations, such as pregnant women and young children.
Recent publications
-
Pharmacokinetic-pharmacodynamic modeling of benznidazole and its antitrypanosomal activity in a murine model of chronic Chagas disease.
Journal article
Assmus F. et al, (2025), PLoS neglected tropical diseases, 19
-
Simplifying medicine dosing for children by harmonising weight bands across therapeutic areas.
Journal article
Waalewijn H. et al, (2025), The Lancet. Child & adolescent health, 9, 274 - 282
-
Dose‐Optimization of a Novel Co‐Formulated Triple Combination Antimalarial Therapy: Artemether‐Lumefantrine‐Amodiaquine
Journal article
Tarning J. et al, (2025), Clinical Pharmacology & Therapeutics
-
A LC‐MS/MS Assay for Quantification of Amodiaquine and Desethylamodiaquine in Dried Blood Spots on Filter Paper
Journal article
Kaewkhao N. et al, (2025), International Journal of Analytical Chemistry, 2025
-
Author Correction: Impact of standard and long-lasting ivermectin formulations in cattle and buffalo on wild Anopheles survival on Sumba Island, Indonesia.
Journal article
Kobylinski KC. et al, (2025), Scientific reports, 15